Many of us get our information about COVID-19 from television, the internet, or social media. We want to know what is going on so that we can make good decisions, and we trust (at least some of the time) that our political leaders and health organizations will protect us.
We also are partially, even secretly, intrigued by the drama of it all. Was the virus a laboratory experiment gone horribly wrong? Is President Donald Trump pitching drugs out of financial interest? Are people actually immune, and can we ever develop a vaccine that would protect us?
Our desire for clear guidance has not been fulfilled, nor has our search for useful data been satisfying. This is partially due to the enormous magnitude of news that bombards us each day. It is also due to the inaccessibility of scientific and academic articles for the general public.

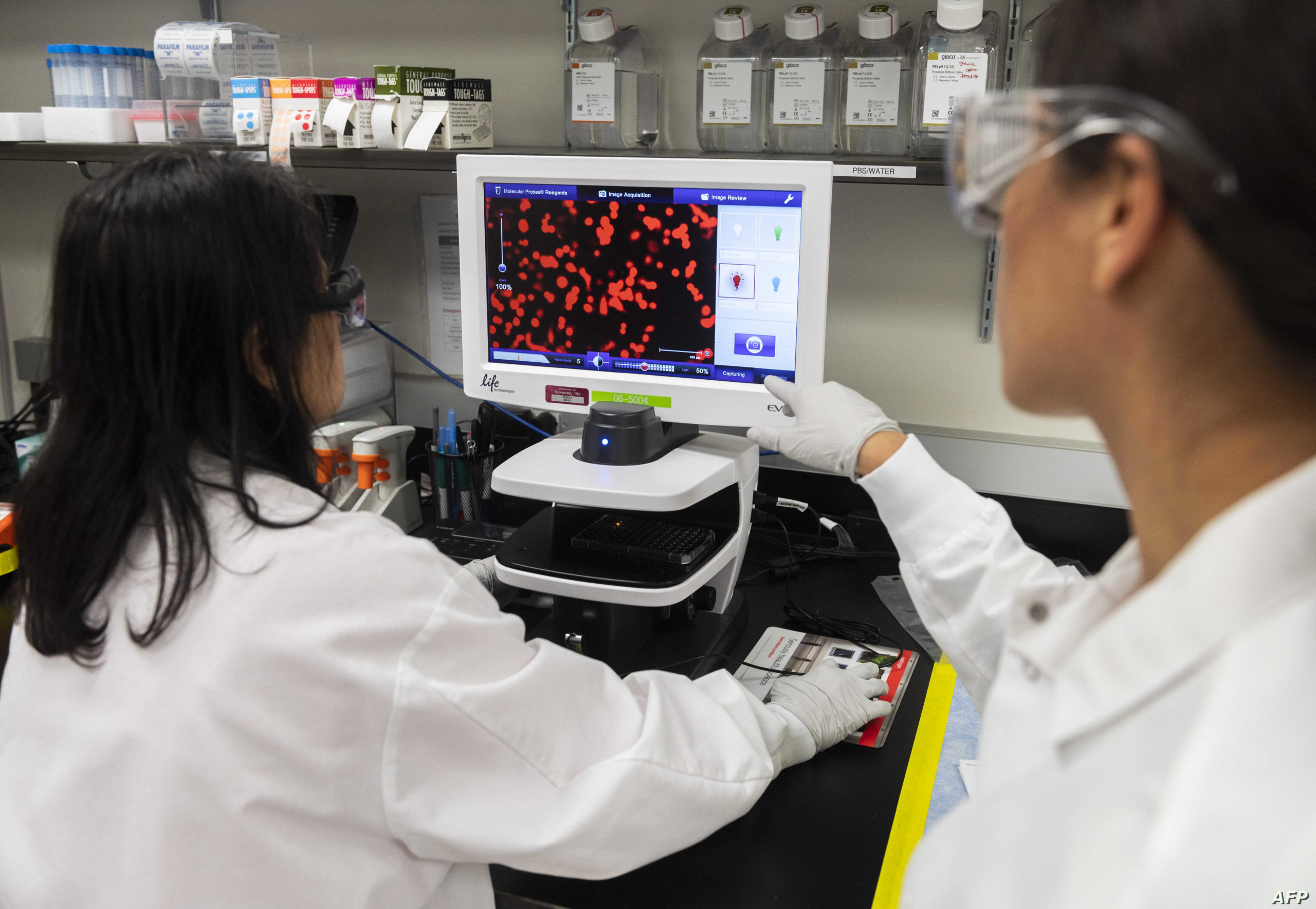
Since January 1, 2020, over 200 scientific articles have been published on the genetics, histology, and immunology of the SARS-CoV-2 virus and COVID-19, the illness caused by the virus.
These articles have been published in reputable journals, and their scientific insights would help inform public policy as well as individuals’ actions. Some of these studies do not have a large sample number, but even these could point us in the right direction of what to research and how to proceed.
The information, however, has not made a great enough impact. It needs to.
Recovered COVID-19 Patients Likely to Be Immune
Last month, the WHO cautioned that currently there is no evidence that individuals who have recovered have sustained immunity. However, absence of evidence does not mean evidence of absence, and a fuller look at the scientific data gives a clearer view of how immunity to COVID-19 works.
From the limited data reported, the genome of SARS-CoV-2 has remained highly stable during its global spread; it hasn’t mutated that much. This suggests that, in general, people would be immune once they caught the virus. It also means that any effective vaccine would provide relatively long-lasting immunity. We can make this assumption based on knowledge of how immunity and vaccines work.
Pfizer and German pharmaceutical company BioNTech say their potential coronavirus vaccine began human trials in the U.S. on Monday. If the tests are successful, the vaccine could be ready for emergency use in September. From the NYT: https://t.co/MGvcTe4fOQ
— Chicago Tribune (@chicagotribune) May 5, 2020
Patients recover from the Sars-CoV-2 infection because their immune systems have produced antibodies that fight the virus. Vaccines essentially introduce the virus into a person’s body in a way that makes producing those antibodies possible. Contrast this to the common cold virus, for example, which mutates rapidly. The continuous mutation of the common cold virus makes it difficult to generate any long-term vaccine. This is why people continue to catch a cold even after they just got over one.
Genetics Help Predict COVID-19 Risk
One scientific study that examined 2,173 patients found that people’s blood type reveals a lot about the person’s risk in contracting COVID-19.
People with blood type A had a significantly higher risk for COVID-19, and people with blood type O had a significantly lower risk. The correlation between blood type and the susceptibility of catching a virus is not unique to SARS-CoV-2.
Genetics may also be important in understanding why there may be a higher chance for older men to die from COVID-19 as opposed to older women. The immune system of older adults undergoes numerous age-related changes that affect immune systems.
Of course, for both the question of immunity and vulnerability more population-based studies are necessary, but this type of research could guide us in how to open up the country again. It can also help us understand why specific populations are more vulnerable so that we can establish public policies that protect the most vulnerable.
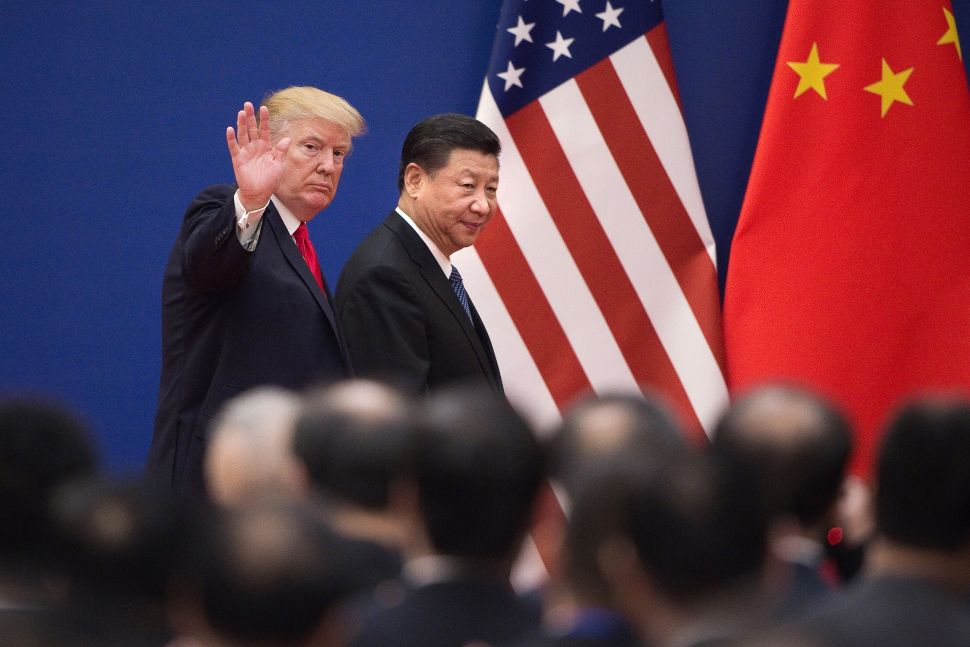
Was COVID-19 Created in a Lab?
Misinformation about this question will affect more than whether and when we can open the country up again. The answer to this question may cause a reevaluation of international alliances and the future of biological warfare. Yet, recent studies have provided support to suggest that SARS‐CoV‐2 is not a lab test gone horribly wrong. Instead, it emerged naturally through genetic recombination of at least two viral strains – a bat β‐coronavirus (β‐CoV) and a pangolin β‐CoV.
Despite various news reports, there is no concrete evidence from any published scientific journal supporting that the virus was generated in a laboratory. Scientists’ ability to correct misinformation and stop conspiracy theories will not only allay fears and anxieties; it could prevent international conflict.
Science and trust in the scientific community have already proven to be the best and fastest way to stop the pandemic and move forward. Over the next months, the scientific community must improve communicating its findings to the general public for all of us to ensure that, even if we disagree on what we should do, we at least agree on the basic facts.
To be able to listen and trust the scientific community, however, we need two essential things. We need to be able to understand what the scientific community has to say. This means that scientists must learn how to share their findings in ways that the public can understand. They need to speak without technical jargon, but in a way that doesn’t simplify too much.
We also need to be able to hear the message over the political noise. This means that scientists must play a civic role that is apolitical. They must inform the public of the data without trying to shape the political agenda.
Disclaimer: The views and opinions expressed here are those of the author and do not necessarily reflect the editorial position of The Globe Post.